SCIENTIFIC PROGRAMME
SESSION I
HOW I TREAT
SMOLDERING MYELOMA
(SMM)
SESSION II
HOW I TREAT NEWLY
DIAGNOSED MULTIPLE
MYELOMA
SESSION III
FROM RISK
STRATIFICATION TO
RISK-BASED THERAPY?
DEBATE 1
SHOULD WE USE MRD
TESTING TO DETERMINE
THERAPY IN MULTIPLE
MYELOMA?
DEBATE 2
IS THERE A FUTURE ROLE
OF AUTOLOGOUS STEM
CELL TRANSPLANTATION?
SESSION IV
HOW I TREAT RELAPSED
MULTIPLE MYELOMA
DEBATE 3
SHOULD EVERY PATIENT
RECEIVE DARATUMUMAB
IN FIRST LINE?
ROUNDTABLE
MULTIPLE MYELOMA
FROM THE PERSPECTIVE
OF FDA/EMEA AND
FOUNDATIONS
SESSION V
YOU CAN’T BE IMMUNE
FOR IMMUNE THERAPY
ANYMORE
SESSION VI
OTHER PLASMA CELL
DYSCRASIAS
KEYNOTE LECTURES
THE FUTURE OF
MULTIPLE MYELOMA
SELECTED ABSTRACTS
FOR AN ORAL
PRESENTATION
ABSTRACTS SELECTED
AS POSTERS
DISCLOSURES
DANIEL AUCAIR (BOSTON)
MYDRUG MASTER PROTOCOL : PRECISION INTERVENTION IN MULTIPLE MYELOMA
Multiple Myeloma Research Foundation, Boston, USA
Multiple myeloma (MM) is the second most prevalent blood cancer, representing approximately 2%
of all cancers. Although overall survival has improved in recent years due to new approved agents (1),
the vast majority of MM patients ultimately stop responding to treatment. Moreover, about a quarter
of MM patients characterized as high risk experience limited benefit from existing treatments (2).
Seminal genomic sequencing research efforts, such as the MMRF CoMMpass study, have highlighted
that a large number of MM cases harbor potentially actionable oncogenic molecular alterations and
published reports on small numbers of cases suggest that Precision interventions clinically targeting
such actionable drivers may benefit MM patients. These results suggest that PM approaches in MM
are possible and should be further studied clinically (3). To that end, we have launched Myeloma-
Developing Regimens Using Genomics (MyDRUG), a master protocol aimed at developing new
myeloma regimens based on individual’s genomics (4).
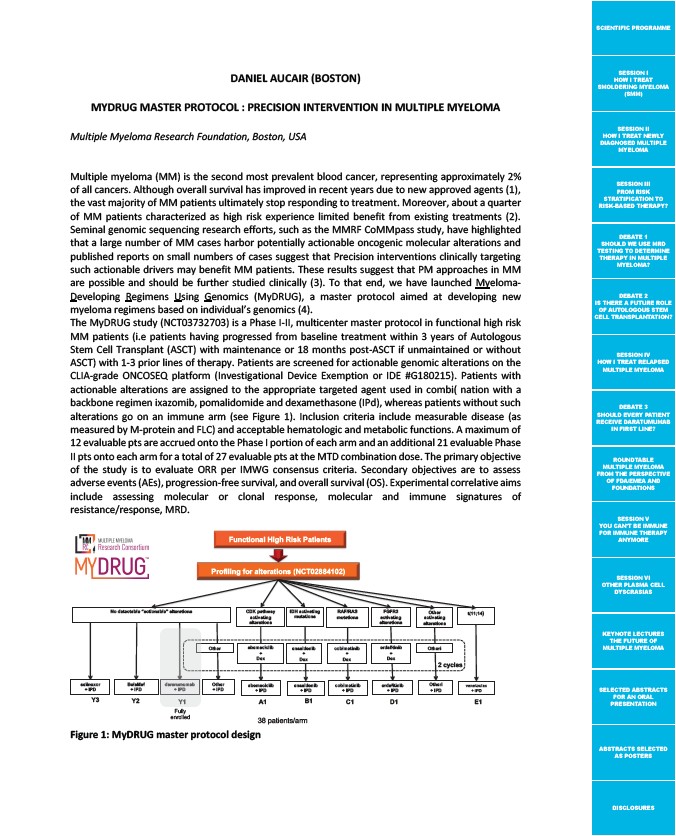
The MyDRUG study (NCT03732703) is a Phase I-II, multicenter master protocol in functional high risk
MM patients (i.e patients having progressed from baseline treatment within 3 years of Autologous
Stem Cell Transplant (ASCT) with maintenance or 18 months post-ASCT if unmaintained or without
ASCT) with 1-3 prior lines of therapy. Patients are screened for actionable genomic alterations on the
CLIA-grade ONCOSEQ platform (Investigational Device Exemption or IDE #G180215). Patients with
actionable alterations are assigned to the appropriate targeted agent used in combi( nation with a
backbone regimen ixazomib, pomalidomide and dexamethasone (IPd), whereas patients without such
alterations go on an immune arm (see Figure 1). Inclusion criteria include measurable disease (as
measured by M-protein and FLC) and acceptable hematologic and metabolic functions. A maximum of
12 evaluable pts are accrued onto the Phase I portion of each arm and an additional 21 evaluable Phase
II pts onto each arm for a total of 27 evaluable pts at the MTD combination dose. The primary objective
of the study is to evaluate ORR per IMWG consensus criteria. Secondary objectives are to assess
adverse events (AEs), progression-free survival, and overall survival (OS). Experimental correlative aims
include assessing molecular or clonal response, molecular and immune signatures of
resistance/response, MRD.
Functional High Risk Patients
CDK pathway
activating
alterations
38 patients/arm
dararumumab
+ IPD
BelaMaf
+ IPD
selinexor
+ IPD
Figure 1: MyDRUG master protocol design
t(11;14)
Profiling for alterations (NCT02884102)
No detectable “actionable” alterations
abemaciclib
+
Dex
abemaciclib
+ IPD
IDH activating
mutations
enasidenib
+
Dex
enasidenib
+ IPD
RAF/RAS
mutations
cobimetinib
+
Dex
cobimetinib
+ IPD
FGFR3
activating
alterations
erdafitinib
+
Dex
erdafitinib
+ IPD
venetoclax
+ IPD
Other
activating
alterations
Otheri
2 cycles
Otheri
+ IPD
Other
Other
+ IPD
Y3 Y2 Y1
A1 B1 C1 D1 E1
Fully
enrolled