SCIENTIFIC PROGRAMME
SESSION I
HOW I TREAT
SMOLDERING MYELOMA
(SMM)
SESSION II
HOW I TREAT NEWLY
DIAGNOSED MULTIPLE
MYELOMA
SESSION III
FROM RISK
STRATIFICATION TO
RISK-BASED THERAPY?
DEBATE 1
SHOULD WE USE MRD
TESTING TO DETERMINE
THERAPY IN MULTIPLE
MYELOMA?
DEBATE 2
IS THERE A FUTURE ROLE
OF AUTOLOGOUS STEM
CELL TRANSPLANTATION?
SESSION IV
HOW I TREAT RELAPSED
MULTIPLE MYELOMA
DEBATE 3
SHOULD EVERY PATIENT
RECEIVE DARATUMUMAB
IN FIRST LINE?
ROUNDTABLE
MULTIPLE MYELOMA
FROM THE PERSPECTIVE
OF FDA/EMEA AND
FOUNDATIONS
SESSION V
YOU CAN’T BE IMMUNE
FOR IMMUNE THERAPY
ANYMORE
SESSION VI
OTHER PLASMA CELL
DYSCRASIAS
KEYNOTE LECTURES
THE FUTURE OF
MULTIPLE MYELOMA
SELECTED ABSTRACTS
FOR AN ORAL
PRESENTATION
ABSTRACTS SELECTED
AS POSTERS
DISCLOSURES POSTER 5
CASTLEMAN DISEASE – A REVIEW OF 8 CASES FROM A SINGLE CENTRE
Sherry Abraham
Regional Cancer Centre, Trivandrum, India
Introduction
Castleman Disease (CD) describes a group of heterogeneous hematologic disorders characterized by
non-neoplastic lymph node hypertrophy and angiofollicular lymph node hyperplasia. Unicentric form
with involvement of a single site is more common than multicentric form. Some are caused by human
herpesvirus-8 (HHV-8) while others are idiopathic. It has been mostly been reported in adults.
Objective
To study the clinical profile and treatment outcome of patients with Castleman disease.
Materials and methods
This is a retrospective study of 8 patients with Castleman disease diagnosed and treated at Regional
Cancer Center, Trivandrum from 2017 to 2019. Data regarding patient’s demographic details, clinical
presentation, histology, staging, treatment and outcome were studied.
Results
The median age was 56.5 years(range 24 to 63 years). There were six males and 2 females. Clinical
presentation, histology and treatment outcome is summarised in table 1. Two patients each presented
with mesenteric mass, retroperitoneal tumour and generalised lymphadenopathy respectively. One
patient each had an ascending colon mass and posterior mediastinal mass. Unicentric CD was
diagnosed in 5 patients and 3 had multicentric disease. Three patients had hyaline vascular subtype of
CD while 2 patients each had plasma cell type and mixed type and in one the subtype was unknown.
All patients were negative for HIV. Human herpes virus(HHV) was negative in 5 patients, while status
was unknown in 3. One patient had associated POEMS syndrome.
Among the patients with unicentric disease, four underwent tumour excision and one underwent
debulking surgery and radiotherapy. Among the patients with multicentric disease, 2 received 4 doses
of single agent rituximab. The other patient was treated with CHOP regime. All patients with unicentric
disease achieved complete remission(CR) and are on regular follow up at 21, 120, 31, 26, 34 months
respectively. Two patients treated with rituximab(#3,#5) had partial response(PR). #5 had disease
progression and received CHOP regime. He has SD(stable disease) and is alive at 28 months follow up.
Patient(#8) with multicentric disease died soon after starting chemotherapy. The median overall
survival(OS) was 28 months(range 21 to 120 months)
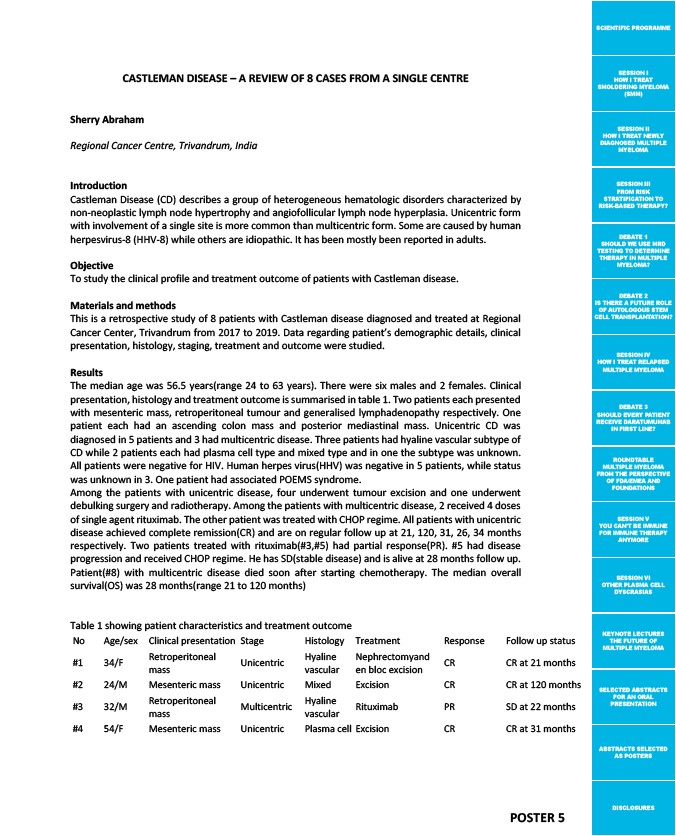
Table 1 showing patient characteristics and treatment outcome
No Age/sex Clinical presentation Stage Histology Treatment Response Follow up status
#1 34/F Retroperitoneal
mass Unicentric Hyaline
vascular
Nephrectomyand
en bloc excision CR CR at 21 months
#2 24/M Mesenteric mass Unicentric Mixed Excision CR CR at 120 months
#3 32/M Retroperitoneal
mass Multicentric Hyaline
vascular Rituximab PR SD at 22 months
#4 54/F Mesenteric mass Unicentric Plasma cell Excision CR CR at 31 months