IMPACT OF RAS-PATHWAY ACTIVATION ON PHENOTYPE AND OUTCOME IN PATIENTS
WITH CHRONIC MYELOMONOCYTIC LEUKEMIA AND A TET2/SRSF2 COMUTATION
Klaus Geissler
Sigmund Freud University, Vienna, Austria
Objectives: In unselected patients with chronic myelomonocytic leukemia (CMML) the prognostic
impact of RAS mutations remains unclear, with some studies, but not all, demonstrating inferior
outcomes (Coltro G and Patnaik MM. Curr Oncol Rep 2019). This fact may be due to variability of the
mutational landscape in patient populations. The combination of TET2 and SRSF2 mutations is very
frequently observed in CMML and highly specific for myeloid neoplasm with monocytosis (Itzykson R
et al, Hemasphere 2019). Therefore we chose this subgroup to analyse the impact of RAS pathway
mutations in a common molecularly defined category of CMML patients.
Methods: 87 of 291 CMML patients in our unselected real world „Austrian Biodatabase for CMML“
(ABCMML) were found to have a TET2/SRSF2 comutation. In 37 of these patients additional mutations
in at least one component of the RAS signaling pathway including NRAS, KRAS, CBL, NF1 and PTPN11,
respectively, were detected.
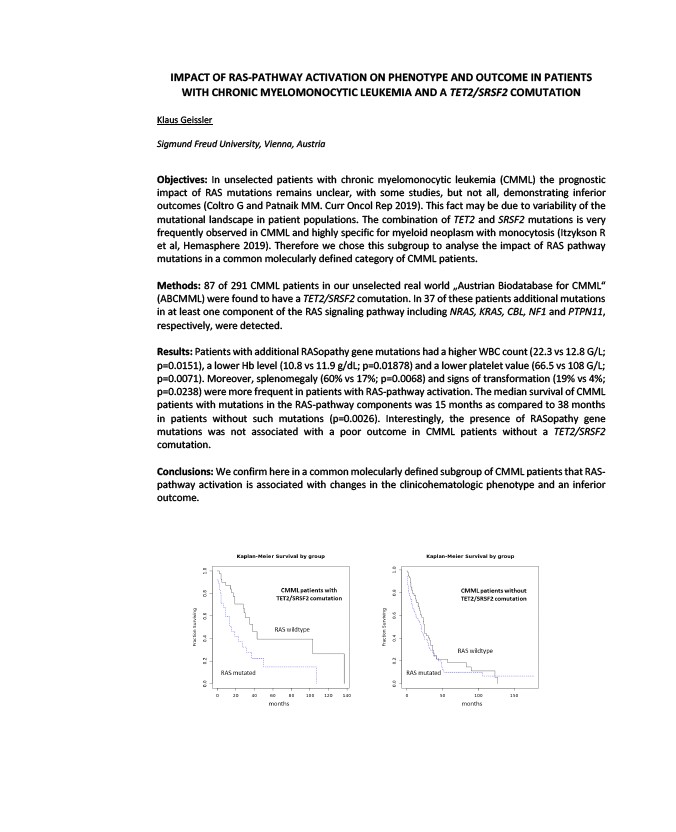
Results: Patients with additional RASopathy gene mutations had a higher WBC count (22.3 vs 12.8 G/L;
p=0.0151), a lower Hb level (10.8 vs 11.9 g/dL; p=0.01878) and a lower platelet value (66.5 vs 108 G/L;
p=0.0071). Moreover, splenomegaly (60% vs 17%; p=0.0068) and signs of transformation (19% vs 4%;
p=0.0238) were more frequent in patients with RAS-pathway activation. The median survival of CMML
patients with mutations in the RAS-pathway components was 15 months as compared to 38 months
in patients without such mutations (p=0.0026). Interestingly, the presence of RASopathy gene
mutations was not associated with a poor outcome in CMML patients without a TET2/SRSF2
comutation.
Conclusions: We confirm here in a common molecularly defined subgroup of CMML patients that RAS-pathway
activation is associated with changes in the clinicohematologic phenotype and an inferior
outcome.