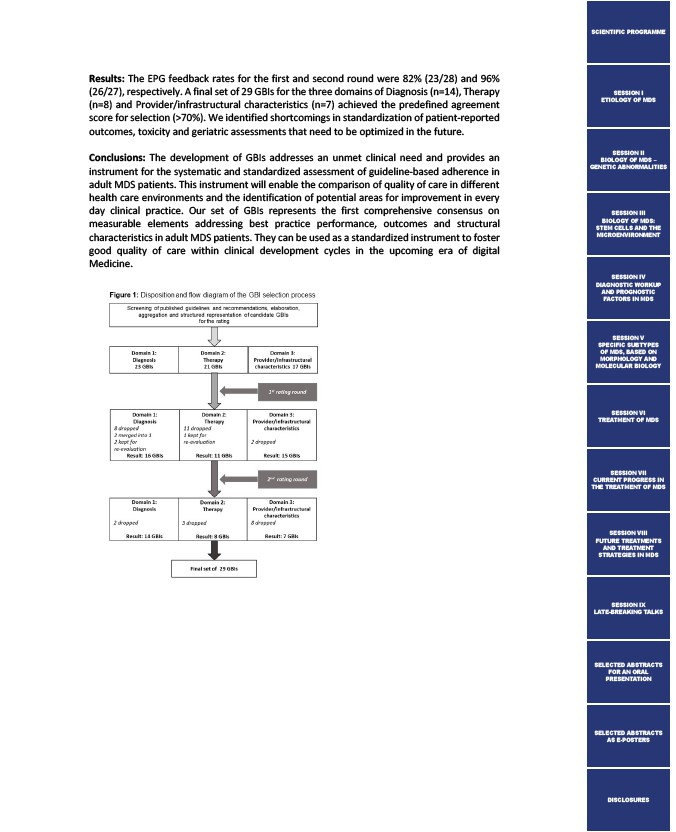
Results: The EPG feedback rates for the first and second round were 82% (23/28) and 96%
(26/27), respectively. A final set of 29 GBIs for the three domains of Diagnosis (n=14), Therapy
(n=8) and Provider/infrastructural characteristics (n=7) achieved the predefined agreement
score for selection (>70%). We identified shortcomings in standardization of patient-reported
outcomes, toxicity and geriatric assessments that need to be optimized in the future.
Conclusions: The development of GBIs addresses an unmet clinical need and provides an
instrument for the systematic and standardized assessment of guideline-based adherence in
adult MDS patients. This instrument will enable the comparison of quality of care in different
health care environments and the identification of potential areas for improvement in every
day clinical practice. Our set of GBIs represents the first comprehensive consensus on
measurable elements addressing best practice performance, outcomes and structural
characteristics in adult MDS patients. They can be used as a standardized instrument to foster
good quality of care within clinical development cycles in the upcoming era of digital
Medicine.
SCIENTIFIC PROGRAMME
SESSION I
ETIOLOGY OF MDS
SESSION II
BIOLOGY OF MDS –
GENETIC ABNORMALITIES
SESSION III
BIOLOGY OF MDS:
STEM CELLS AND THE
MICROENVIRONMENT
SESSION IV
DIAGNOSTIC WORKUP
AND PROGNOSTIC
FACTORS IN MDS
SESSION V
SPECIFIC SUBTYPES
OF MDS, BASED ON
MORPHOLOGY AND
MOLECULAR BIOLOGY
SESSION VI
TREATMENT OF MDS
SESSION VII
CURRENT PROGRESS IN
THE TREATMENT OF MDS
SESSION VIII
FUTURE TREATMENTS
AND TREATMENT
STRATEGIES IN MDS
SESSION IX
LATE-BREAKING TALKS
SELECTED ABSTRACTS
FOR AN ORAL
PRESENTATION
SELECTED ABSTRACTS
AS E-POSTERS
DISCLOSURES