POSTER 35
AN UNUSUAL CASE OF MEGAKARYOCYTIC BLAST CRISIS OF CHRONIC
MYELOID LEUKEMIA
Abibatou Sall, Moussa Seck, Blaise Félix Faye, Macoura Gadji, Saliou Diop and Awa Oumar Touré
Hematology, Cheikh Anta Diop University, Dakar, Senegal
A 59-year-old Senegalese woman with a past medical story of chronic myeloid leukemia (CML),
BCR-ABL positive, diagnosed 2 years ago and under Dasatinib, was referred to our hospital for
disorientation and fever. Physical examination revealed splenomegaly type2, pallor and
petechiae in her lower limbs.
The blood count showed severe normocytic normochromic anemia: Hb=58g/L and MCV =
90FL; high leukocytosis (405 × 109/L) and low platelet count (89 × 109/L).
Blood examination showed hyper cellularity with marked increase in mature neutrophil
granulocytes and their precursors. However, we did not find the 2 peaks of myelocytes and
neutrophils as found in the chronic form of CML. Myeloblast count was 7% and promyelocytes
8%. The megakaryocytic lineage was present in the blood film with very atypical morphology.
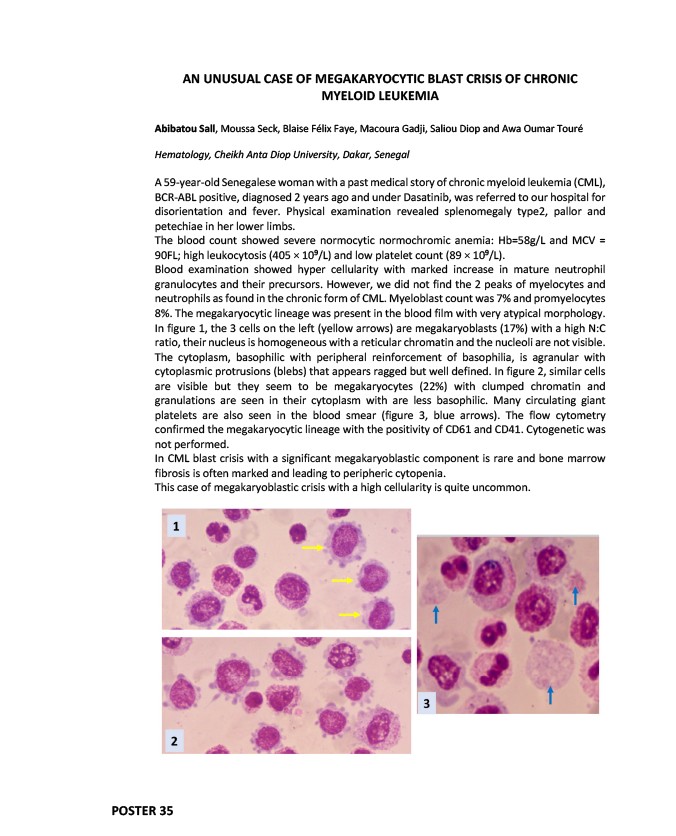
In figure 1, the 3 cells on the left (yellow arrows) are megakaryoblasts (17%) with a high N:C
ratio, their nucleus is homogeneous with a reticular chromatin and the nucleoli are not visible.
The cytoplasm, basophilic with peripheral reinforcement of basophilia, is agranular with
cytoplasmic protrusions (blebs) that appears ragged but well defined. In figure 2, similar cells
are visible but they seem to be megakaryocytes (22%) with clumped chromatin and
granulations are seen in their cytoplasm with are less basophilic. Many circulating giant
platelets are also seen in the blood smear (figure 3, blue arrows). The flow cytometry
confirmed the megakaryocytic lineage with the positivity of CD61 and CD41. Cytogenetic was
not performed.
In CML blast crisis with a significant megakaryoblastic component is rare and bone marrow
fibrosis is often marked and leading to peripheric cytopenia.
This case of megakaryoblastic crisis with a high cellularity is quite uncommon.